
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Basic Research
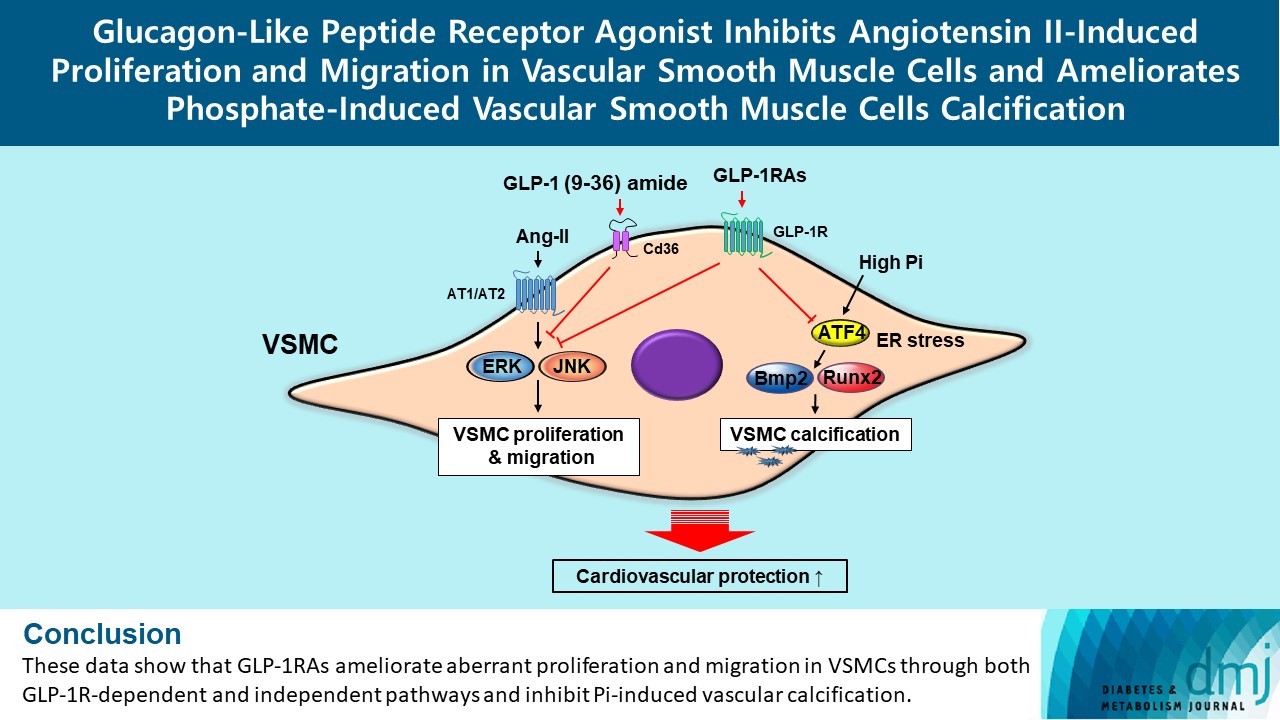
- Glucagon-Like Peptide Receptor Agonist Inhibits Angiotensin II-Induced Proliferation and Migration in Vascular Smooth Muscle Cells and Ameliorates Phosphate-Induced Vascular Smooth Muscle Cells Calcification
- Jinmi Lee, Seok-Woo Hong, Min-Jeong Kim, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
- Diabetes Metab J. 2024;48(1):83-96. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0363
- 1,726 View
- 168 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Glucagon-like peptide-1 receptor agonist (GLP-1RA), which is a therapeutic agent for the treatment of type 2 diabetes mellitus, has a beneficial effect on the cardiovascular system.
Methods
To examine the protective effects of GLP-1RAs on proliferation and migration of vascular smooth muscle cells (VSMCs), A-10 cells exposed to angiotensin II (Ang II) were treated with either exendin-4, liraglutide, or dulaglutide. To examine the effects of GLP-1RAs on vascular calcification, cells exposed to high concentration of inorganic phosphate (Pi) were treated with exendin-4, liraglutide, or dulaglutide.
Results
Ang II increased proliferation and migration of VSMCs, gene expression levels of Ang II receptors AT1 and AT2, proliferation marker of proliferation Ki-67 (Mki-67), proliferating cell nuclear antigen (Pcna), and cyclin D1 (Ccnd1), and the protein expression levels of phospho-extracellular signal-regulated kinase (p-Erk), phospho-c-JUN N-terminal kinase (p-JNK), and phospho-phosphatidylinositol 3-kinase (p-Pi3k). Exendin-4, liraglutide, and dulaglutide significantly decreased the proliferation and migration of VSMCs, the gene expression levels of Pcna, and the protein expression levels of p-Erk and p-JNK in the Ang II-treated VSMCs. Erk inhibitor PD98059 and JNK inhibitor SP600125 decreased the protein expression levels of Pcna and Ccnd1 and proliferation of VSMCs. Inhibition of GLP-1R by siRNA reversed the reduction of the protein expression levels of p-Erk and p-JNK by exendin-4, liraglutide, and dulaglutide in the Ang II-treated VSMCs. Moreover, GLP-1 (9-36) amide also decreased the proliferation and migration of the Ang II-treated VSMCs. In addition, these GLP-1RAs decreased calcium deposition by inhibiting activating transcription factor 4 (Atf4) in Pi-treated VSMCs.
Conclusion
These data show that GLP-1RAs ameliorate aberrant proliferation and migration in VSMCs through both GLP-1Rdependent and independent pathways and inhibit Pi-induced vascular calcification. -
Citations
Citations to this article as recorded by- Incretin Hormone Secretion in Women with Polycystic Ovary Syndrome: Roles of Obesity, Insulin Sensitivity and Treatment with Metformin and GLP-1s
Andrea Etrusco, Mislav Mikuš, Antonio D’Amato, Fabio Barra, Petar Planinić, Trpimir Goluža, Giovanni Buzzaccarini, Jelena Marušić, Mara Tešanović, Antonio Simone Laganà
Biomedicines.2024; 12(3): 653. CrossRef
- Incretin Hormone Secretion in Women with Polycystic Ovary Syndrome: Roles of Obesity, Insulin Sensitivity and Treatment with Metformin and GLP-1s
- Lifestyle
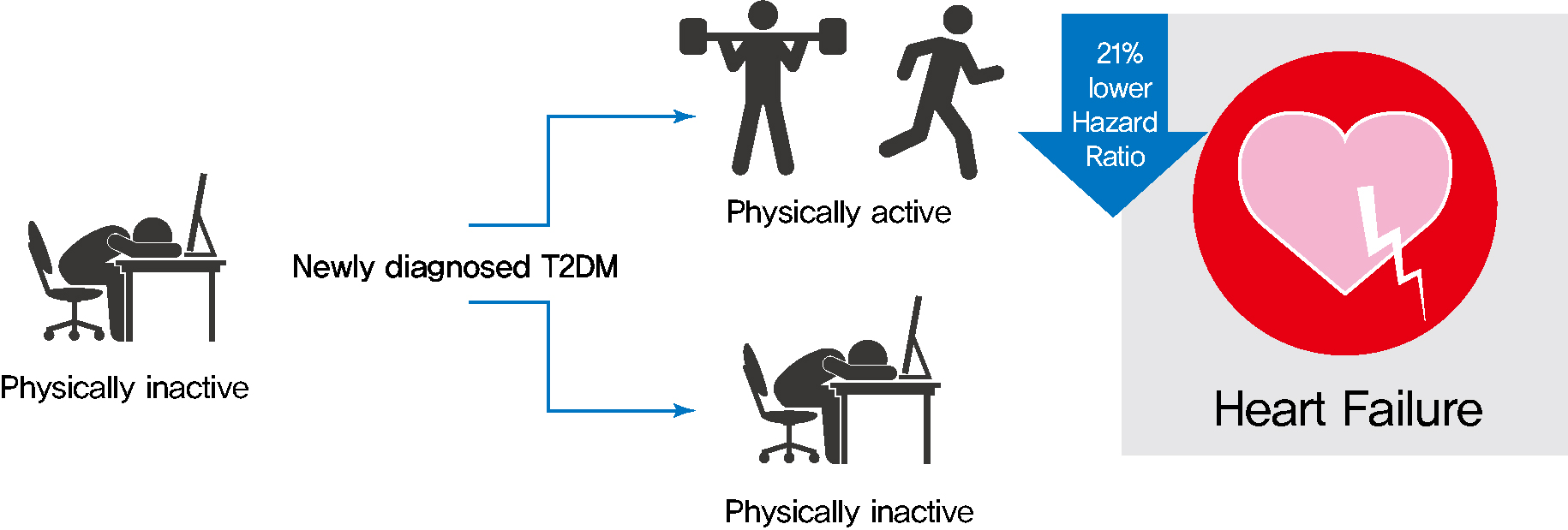
- Changes in Patterns of Physical Activity and Risk of Heart Failure in Newly Diagnosed Diabetes Mellitus Patients
- Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
- Diabetes Metab J. 2022;46(2):327-336. Published online November 24, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0046
- 5,406 View
- 210 Download
- 4 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 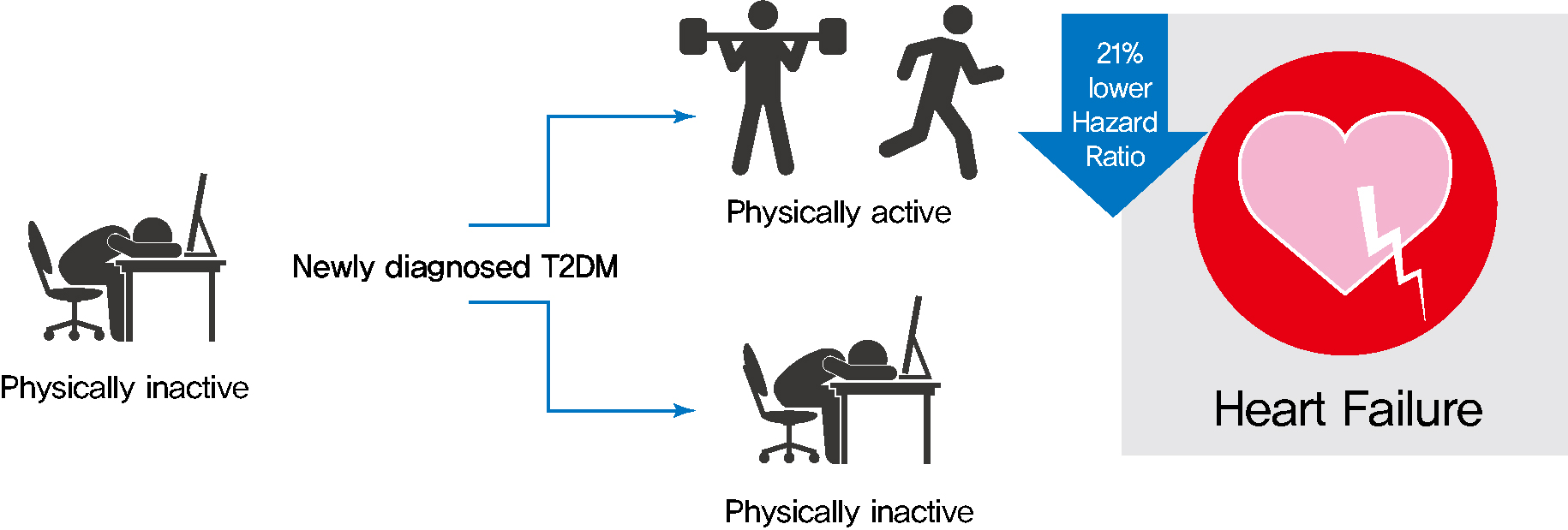
- Background
Exercise is recommended for type 2 diabetes mellitus (T2DM) patients to prevent cardiovascular disease. However, the effects of physical activity (PA) for reducing the risk of heart failure (HF) has yet to be elucidated. We aimed to assess the effect of changes in patterns of PA on incident HF, especially in newly diagnosed diabetic patients.
Methods
We examined health examination data and claims records of 294,528 participants from the Korean National Health Insurance Service who underwent health examinations between 2009 and 2012 and were newly diagnosed with T2DM. Participants were classified into the four groups according to changes in PA between before and after the diagnosis of T2DM: continuously inactive, inactive to active, active to inactive, and continuously active. The development of HF was analyzed until 2017.
Results
As compared with those who were continuously inactive, those who became physically active after diagnosis showed a reduced risk for HF (adjusted hazard ratio [aHR], 0.79; 95% confidence interval [CI], 0.66 to 0.93). Those who were continuously active had the lowest risk for HF (aHR, 0.77; 95% CI, 0.62 to 0.96). As compared with those who were inactive, those who exercised regularly, either performing vigorous or moderate PA, had a lower HF risk (aHR, 0.79; 95% CI, 0.69 to 0.91).
Conclusion
Among individuals with newly diagnosed T2DM, the risk of HF was reduced in those with higher levels of PA after diagnosis was made. Our results suggest either increasing or maintaining the frequency of PA after the diagnosis of T2DM may lower the risk of HF. -
Citations
Citations to this article as recorded by- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study
Kyoung Min Kim, Kyoung Jin Kim, Kyungdo Han, Yumie Rhee
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1194. CrossRef - Evaluation and Management of Patients With Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
International Journal of Heart Failure.2023; 5(1): 1. CrossRef - Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 10. CrossRef - Association of plasma brain-derived neurotrophic factor levels and frailty in community-dwelling older adults
Eun Roh, Soon Young Hwang, Eyun Song, Min Jeong Park, Hye Jin Yoo, Sei Hyun Baik, Miji Kim, Chang Won Won, Kyung Mook Choi
Scientific Reports.2022;[Epub] CrossRef - The associations between changes in hepatic steatosis and heart failure and mortality: a nationwide cohort study
Jiyun Park, Gyuri Kim, Hasung Kim, Jungkuk Lee, Sang-Man Jin, Jae Hyeon Kim
Cardiovascular Diabetology.2022;[Epub] CrossRef
- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study
- Metabolic Risk/Epidemiology
- Dose-Dependent Effect of Smoking on Risk of Diabetes Remains after Smoking Cessation: A Nationwide Population-Based Cohort Study in Korea
- Se Eun Park, Mi Hae Seo, Jung-Hwan Cho, Hyemi Kwon, Yang-Hyun Kim, Kyung-Do Han, Jin-Hyung Jung, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
- Diabetes Metab J. 2021;45(4):539-546. Published online March 4, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0061
- 7,721 View
- 188 Download
- 9 Web of Science
- 12 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 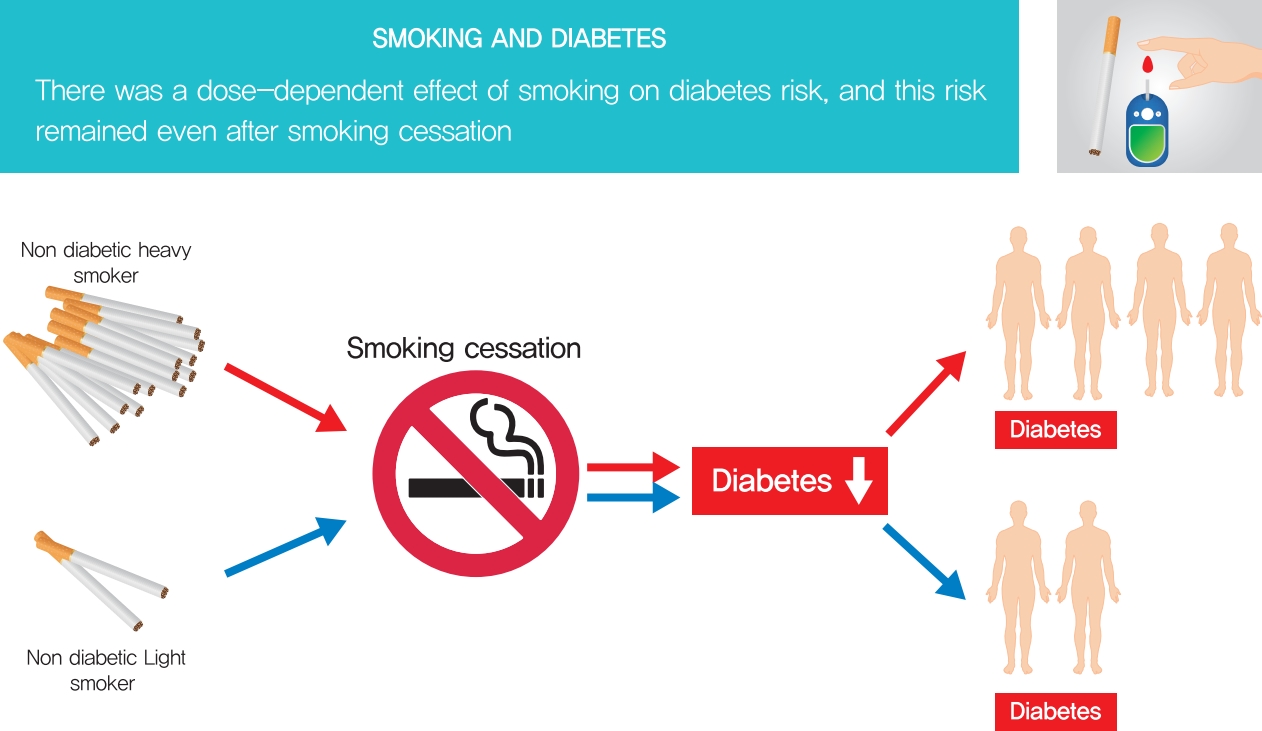
- Background
This study aimed to evaluate the dose-dependent effects of smoking on risk of diabetes among those quitting smoking.
Methods
We analyzed clinical data from a total of 5,198,792 individuals age 20 years or older who received health care check-up arranged by the national insurance program of Korea between 2009 and 2016 using the Korean National Health Insurance Service database. Cumulative smoking was estimated by pack-years. Smokers were classified into four categories according to the amount of smoking: light smokers (0.025 to 5 smoking pack-years), medium smokers (5 to 14 smoking pack-years), heavy smokers (14 to 26 smoking pack-years), and extreme smokers (more than 26 smoking pack-years).
Results
During the study period, 164,335 individuals (3.2% of the total population) developed diabetes. Compared to sustained smokers, the risk of diabetes was significantly reduced in both quitters (hazard ratio [HR], 0.858; 95% confidence interval [CI], 0.838 to 0.878) and nonsmokers (HR, 0.616; 95% CI, 0.606 to 0.625) after adjustment for multiple risk factors. The risk of diabetes gradually increased with amount of smoking in both quitters and current smokers. The risk of diabetes in heavy (HR, 1.119; 95% CI, 1.057 to 1.185) and extreme smokers (HR, 1.348; 95% CI, 1.275 to 1.425) among quitters was much higher compared to light smokers among current smokers.
Conclusion
Smoking cessation was effective in reducing the risk of diabetes regardless of weight change. However, there was a potential dose-dependent association between smoking amount and the development of diabetes. Diabetes risk still remained in heavy and extreme smokers even after smoking cessation. -
Citations
Citations to this article as recorded by- Dietary and other lifestyle factors and their influence on non-communicable diseases in the Western Pacific region
Xiaomin Sun, Dong Keon Yon, Tuan Thanh Nguyen, Kumpei Tanisawa, Kumhee Son, Ling Zhang, Jing Shu, Wen Peng, Yuexin Yang, Francesco Branca, Mark L. Wahlqvist, Hyunjung Lim, Youfa Wang
The Lancet Regional Health - Western Pacific.2024; 43: 100842. CrossRef - The Concentrations of Interleukin-6, Insulin, and Glucagon in the Context of Obesity and Type 2 Diabetes and Single Nucleotide Polymorphisms in IL6 and INS Genes
Magdalena Król-Kulikowska, Iwona Urbanowicz, Marta Kepinska, Mayank Choubey
Journal of Obesity.2024; 2024: 1. CrossRef - Chronic cigarette smoking is associated with increased arterial stiffness in men and women: evidence from a large population-based cohort
Omar Hahad, Volker H. Schmitt, Natalie Arnold, Karsten Keller, Jürgen H. Prochaska, Philipp S. Wild, Andreas Schulz, Karl J. Lackner, Norbert Pfeiffer, Irene Schmidtmann, Matthias Michal, Jörn M. Schattenberg, Oliver Tüscher, Andreas Daiber, Thomas Münzel
Clinical Research in Cardiology.2023; 112(2): 270. CrossRef - Association between Meal Frequency and Type 2 Diabetes Mellitus in Rural Adults: A Large-Scale Cross-Sectional Study
Bota Baheti, Xiaotian Liu, Mu Wang, Caiyun Zhang, Xiaokang Dong, Ning Kang, Linlin Li, Xing Li, Songcheng Yu, Jian Hou, Zhenxing Mao, Chongjian Wang
Nutrients.2023; 15(6): 1348. CrossRef - Impaired Lung Function and Lung Cancer Incidence: A Nationwide Population-Based Cohort Study
Hye Seon Kang, Yong-Moon Park, Seung-Hyun Ko, Seung Hoon Kim, Shin Young Kim, Chi Hong Kim, Kyungdo Han, Sung Kyoung Kim
Journal of Clinical Medicine.2022; 11(4): 1077. CrossRef - Smoking cessation and risk of type 2 diabetes
Jana Malinovská, Jana Urbanová, Veronika Vejtasová, Alexandra Romanová, Sabina Pálová, Syed Taha Naeem, Jan Brož
Vnitřní lékařství.2022; 68(1): E04. CrossRef - Association between lung function and the risk of atrial fibrillation in a nationwide population cohort study
Su Nam Lee, Seung-Hyun Ko, Sung-Ho Her, Kyungdo Han, Donggyu Moon, Sung Kyoung Kim, Ki-Dong Yoo, Yu-Bae Ahn
Scientific Reports.2022;[Epub] CrossRef - Sex differences in factors associated with prediabetes in Korean adults
Jin Suk Ra
Osong Public Health and Research Perspectives.2022; 13(2): 142. CrossRef - Smoking and diabetes interplay: A comprehensive review and joint statement
Vincent Durlach, Bruno Vergès, Abdallah Al-Salameh, Thibault Bahougne, Farid Benzerouk, Ivan Berlin, Carole Clair, Jacques Mansourati, Alexia Rouland, Daniel Thomas, Philippe Thuillier, Blandine Tramunt, Anne-Laurence Le Faou
Diabetes & Metabolism.2022; 48(6): 101370. CrossRef - Impact of healthy lifestyle on the risk of type 2 diabetes mellitus in southwest China: A prospective cohort study
Yanli Wu, Xi He, Jie Zhou, Yiying Wang, Lisha Yu, Xuejiao Li, Tao Liu, Jianhua Luo
Journal of Diabetes Investigation.2022; 13(12): 2091. CrossRef - Current status of health promotion in Korea
Soo Young Kim
Journal of the Korean Medical Association.2022; 65(12): 776. CrossRef - Smoking Cessation after Diagnosis of New-Onset Atrial Fibrillation and the Risk of Stroke and Death
So-Ryoung Lee, Eue-Keun Choi, Jin-Hyung Jung, Kyung-Do Han, Seil Oh, Gregory Y. H. Lip
Journal of Clinical Medicine.2021; 10(11): 2238. CrossRef
- Dietary and other lifestyle factors and their influence on non-communicable diseases in the Western Pacific region
- Cardiovascular risk/Epidemiology
- Increased Risk of Cardiovascular Disease and Mortality in Patients with Diabetes and Coexisting Depression: A Nationwide Population-Based Cohort Study
- Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Yang-Hyun Kim, Eun-Jung Rhee, Won-Young Lee
- Diabetes Metab J. 2021;45(3):379-389. Published online December 11, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0008
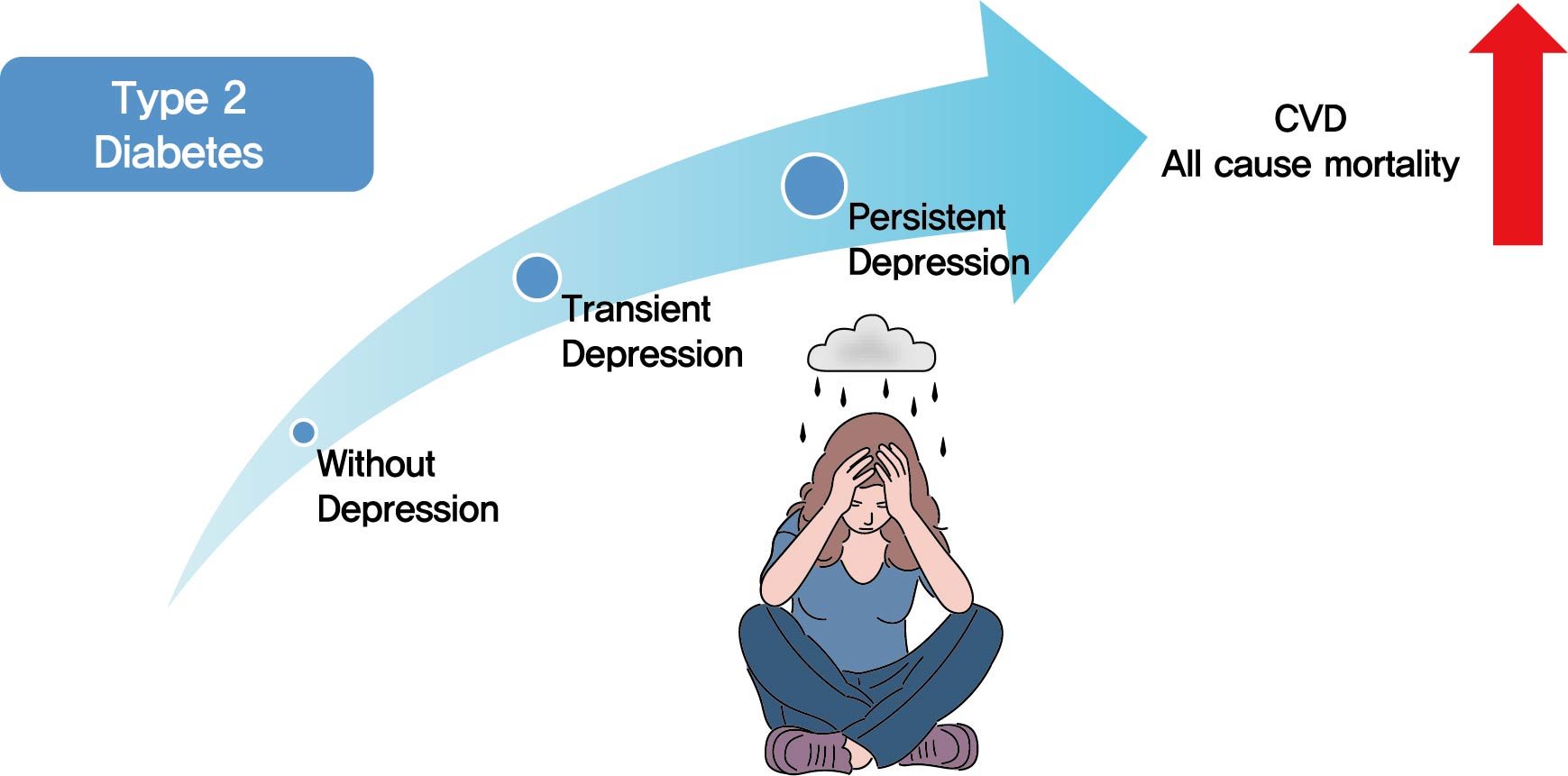
- 7,513 View
- 236 Download
- 22 Web of Science
- 21 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 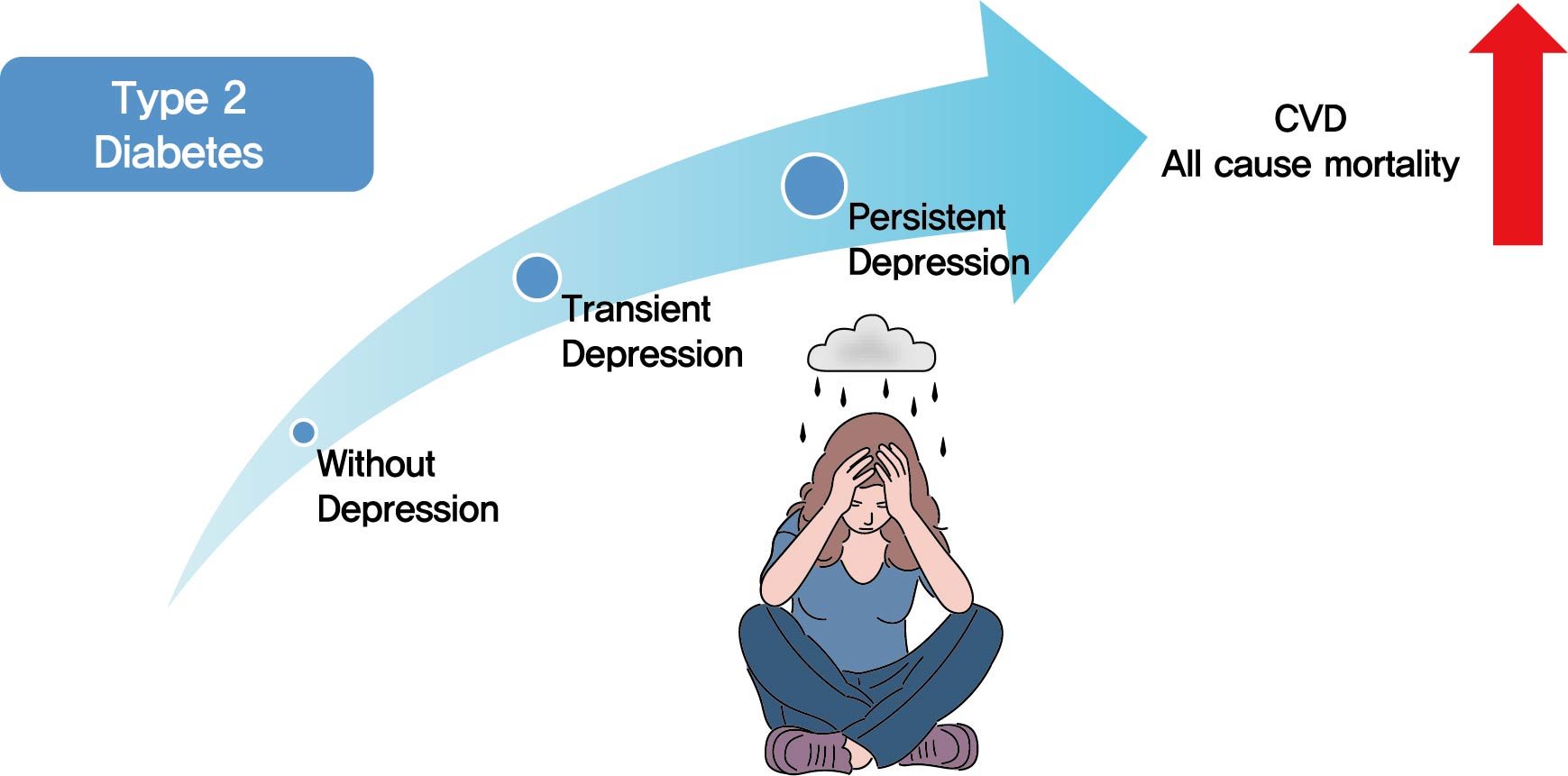
- Background
Previous studies have suggested that depression in patients with diabetes is associated with worse health outcomes. The aim of this study was to evaluate the risk of cardiovascular disease (CVD) and mortality in patients with diabetes with comorbid depression.
Methods
We examined the general health check-up data and claim database of the Korean National Health Insurance Service (NHIS) of 2,668,615 participants with type 2 diabetes mellitus who had examinations between 2009 and 2012. As NHIS database has been established since 2002, those who had been diagnosed with depression or CVD since 2002 were excluded. The 2,228,443 participants were classified into three groups according to the claim history of depression; normal group (n=2,166,979), transient depression group (one episode of depression, n=42,124) and persistent depression group (at least two episodes of depression, n=19,340). The development of CVD and mortality were analyzed from 2009 to 2017.
Results
Those with depression showed a significantly increased risk for stroke (transient depression group: hazard ratio [HR], 1.20; 95% confidence interval [CI], 1.15 to 1.26) (persistent depression group: HR, 1.54; 95% CI, 1.46 to 1.63). Those with depression had an increased risk for myocardial infarction (transient depression group: HR, 1.25; 95% CI, 1.18 to 1.31) (persistent depression group: HR, 1.38; 95% CI, 1.29 to 1.49). The persistent depression group had an increased risk for all-cause mortality (HR, 1.66; 95% CI, 1.60 to 1.72).
Conclusion
Coexisting depression in patients with diabetes has a deleterious effect on the development of CVD and mortality. We suggest that more attention should be given to patients with diabetes who present with depressive symptoms. -
Citations
Citations to this article as recorded by- Psychological resilience mediates the relationship between diabetes distress and depression among persons with diabetes in a multi-group analysis
Ajele Kenni Wojujutari, Erhabor Sunday Idemudia, Lawrence Ejike Ugwu
Scientific Reports.2024;[Epub] CrossRef - The mediating effect of depression on new-onset stroke in diabetic population: Evidence from the China health and retirement longitudinal study
Gege Jiang, Yaoling Wang, Liping Wang, Minfang Chen, Wei Li
Journal of Affective Disorders.2023; 321: 208. CrossRef - Frailty and outcomes in lacunar stroke
Sima Vazquez, Zehavya Stadlan, Justin M Lapow, Eric Feldstein, Smit Shah, Ankita Das, Alexandria F Naftchi, Eris Spirollari, Akash Thaker, Syed Faraz Kazim, Jose F Dominguez, Neisha Patel, Christeena Kurian, Ji Chong, Stephan A Mayer, Gurmeen Kaur, Chirag
Journal of Stroke and Cerebrovascular Diseases.2023; 32(2): 106942. CrossRef - Comparison of Operational Definition of Type 2 Diabetes Mellitus Based on Data from Korean National Health Insurance Service and Korea National Health and Nutrition Examination Survey
Jong Ha Baek, Yong-Moon Park, Kyung Do Han, Min Kyong Moon, Jong Han Choi, Seung-Hyun Ko
Diabetes & Metabolism Journal.2023; 47(2): 201. CrossRef - The Association between Dietary Carotenoid Intake and Risk of Depression among Patients with Cardiometabolic Disease
Jie Liang, Yuhao Wang, Min Chen
International Heart Journal.2023; 64(2): 223. CrossRef - Associations of concomitant retinopathy and depression with mortality in a nationally representative population
Zheng Lyu, Yilin Chen, Zhuoting Zhu, Xiaoyang Luo, Ying Cui, Jie Xie, Zhifan Chen, Junbin Liu, Xiyu Wu, Gabrella Bulloch, Qianli Meng
Journal of Affective Disorders.2023; 336: 15. CrossRef - Clinical insights into the cross-link between mood disorders and type 2 diabetes: A review of longitudinal studies and Mendelian randomisation analyses
Chiara Possidente, Giuseppe Fanelli, Alessandro Serretti, Chiara Fabbri
Neuroscience & Biobehavioral Reviews.2023; 152: 105298. CrossRef - Prevalence of depression and association with all-cause and cardiovascular mortality among individuals with type 2 diabetes: a cohort study based on NHANES 2005–2018 data
Zhen Feng, Wai Kei Tong, Xinyue Zhang, Zhijia Tang
BMC Psychiatry.2023;[Epub] CrossRef - Cholecystectomy Increases the Risk of Type 2 Diabetes in the Korean Population
Ji Hye Huh, Kyong Joo Lee, Yun Kyung Cho, Shinje Moon, Yoon Jung Kim, Eun Roh, Kyung-do Han, Dong Hee Koh, Jun Goo Kang, Seong Jin Lee, Sung-Hee Ihm
Annals of Surgery.2023; 278(2): e264. CrossRef - Risk of depression in patients with acromegaly in Korea (2006-2016): a nationwide population-based study
Shinje Moon, Sangmo Hong, Kyungdo Han, Cheol-Young Park
European Journal of Endocrinology.2023; 189(3): 363. CrossRef - The association between cardiovascular drugs and depression/anxiety in patients with cardiovascular disease: A meta-analysis
Lijun Zhang, Yanping Bao, Shuhui Tao, Yimiao Zhao, Meiyan Liu
Pharmacological Research.2022; 175: 106024. CrossRef - Association of mental health with the risk of coronary artery disease in patients with diabetes: A mendelian randomization study
Teng Hu, Fangkun Yang, Kewan He, Jiajun Ying, Hanbin Cui
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(3): 703. CrossRef - Comorbidity of Type 2 Diabetes Mellitus and Depression: Clinical Evidence and Rationale for the Exacerbation of Cardiovascular Disease
Mengmeng Zhu, Yiwen Li, Binyu Luo, Jing Cui, Yanfei Liu, Yue Liu
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Understanding and Utilizing Claim Data from the Korean National Health Insurance Service (NHIS) and Health Insurance Review & Assessment (HIRA) Database for Research
Dae-Sung Kyoung, Hun-Sung Kim
Journal of Lipid and Atherosclerosis.2022; 11(2): 103. CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - Evaluation of rosmarinic acid against myocardial infarction in maternally separated rats
Himanshu Verma, Anindita Bhattacharjee, Naveen Shivavedi, Prasanta Kumar Nayak
Naunyn-Schmiedeberg's Archives of Pharmacology.2022; 395(10): 1189. CrossRef - Lipid cutoffs for increased cardiovascular disease risk in non-diabetic young people
Mee Kyoung Kim, Kyungdo Han, Hun-Sung Kim, Kun-Ho Yoon, Seung-Hwan Lee
European Journal of Preventive Cardiology.2022; 29(14): 1866. CrossRef - Risk factors associated with mortality among individuals with type 2 diabetes and depression across two cohorts
Christopher Rohde, Jens Steen Nielsen, Jakob Schöllhammer Knudsen, Reimar Wernich Thomsen, Søren Dinesen Østergaard
European Journal of Endocrinology.2022; 187(4): 567. CrossRef - Increased Risk of Cardiovascular Disease and Mortality in Patients with Diabetes and Coexisting Depression: A Nationwide Population-Based Cohort Study (Diabetes Metab J 2021;45:379-89)
Jin Hwa Kim
Diabetes & Metabolism Journal.2021; 45(5): 789. CrossRef - Increased Risk of Cardiovascular Disease and Mortality in Patients with Diabetes and Coexisting Depression: A Nationwide Population-Based Cohort Study (Diabetes Metab J 2021;45:379-89)
Inha Jung, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2021; 45(5): 793. CrossRef - Affective Temperament and Glycemic Control – The Psychological Aspect of Obesity and Diabetes Mellitus
Natalia Lesiewska, Anna Kamińska, Roman Junik, Magdalena Michalewicz, Bartłomiej Myszkowski, Alina Borkowska, Maciej Bieliński
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 4981. CrossRef
- Psychological resilience mediates the relationship between diabetes distress and depression among persons with diabetes in a multi-group analysis
- Associations among Obesity Degree, Glycemic Status, and Risk of Heart Failure in 9,720,220 Korean Adults
- Eun Jung Rhee, Hyemi Kwon, Se Eun Park, Kyung Do Han, Yong Gyu Park, Yang Hyun Kim, Won Young Lee
- Diabetes Metab J. 2020;44(5):783-783. Published online October 21, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0245
- Corrects: Diabetes Metab J 2020;44(4):592

- 3,951 View
- 94 Download
- Cardiovascular Risk/Epidemiology
-
- Associations among Obesity Degree, Glycemic Status, and Risk of Heart Failure in 9,720,220 Korean Adults
- Eun-Jung Rhee, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Yang-Hyun Kim, Won-Young Lee
- Diabetes Metab J. 2020;44(4):592-601. Published online April 20, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0104
- Correction in: Diabetes Metab J 2020;44(5):783

- 6,650 View
- 142 Download
- 16 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background Recent studies suggest an association between diabetes and increased risk of heart failure (HF). However, the associations among obesity status, glycemic status, and risk of HF are not known. In this study, we analyzed whether the risk of HF increases in participants according to baseline glycemic status and whether this increased risk is associated with obesity status.
Methods We analyzed the risk of HF according to baseline glycemic status (normoglycemia, impaired fasting glucose [IFG], and diabetes) in 9,720,220 Koreans who underwent Korean National Health Screening in 2009 without HF at baseline with a median follow-up period of 6.3 years. The participants were divided into five and six groups according to baseline body mass index (BMI) and waist circumference, respectively.
Results Participants with IFG and those with diabetes showed a 1.08- and 1.86-fold increased risk of HF, respectively, compared to normoglycemic participants. Compared to the normal weight group (BMI, 18.5 to 22.9 kg/m2), the underweight group (BMI <18.5 kg/m2) showed a 1.7-fold increased risk of HF, and those with BMI ≥30 kg/m2 showed a 1.1-fold increased risk of HF, suggesting a J-shaped association with BMI. When similar analyses were performed for different glycemic statuses, the J-shaped association between BMI and HF risk was consistently observed in both groups with and without diabetes.
Conclusion Participants with IFG and diabetes showed a significantly increased HF risk compared to normoglycemic participants. This increased risk of HF was mostly prominent in underweight and class II obese participants than in participants with normal weight.
-
Citations
Citations to this article as recorded by- Association between underweight and risk of heart failure in diabetes patients
Tae Kyung Yoo, Kyung‐Do Han, Eun‐Jung Rhee, Won‐Young Lee
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(2): 671. CrossRef - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Research on obesity using the National Health Information Database: recent trends
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 35. CrossRef - Impact of mental disorders on the risk of heart failure among Korean patients with diabetes: a cohort study
Tae Kyung Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Diabetology.2023;[Epub] CrossRef - Differential Impact of Obesity on the Risk of Diabetes Development in Two Age Groups: Analysis from the National Health Screening Program
Tae Kyung Yoo, Kyung-Do Han, Yang-Hyun Kim, Ga Eun Nam, Sang Hyun Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2023; 47(6): 846. CrossRef - Characterization of the oxidative stress and inflammatory markers in metabolically healthy obese individuals
Hazhmat Ali
Al-Kufa University Journal for Biology.2023; 15(3): 28. CrossRef - The Influence of Obesity and Metabolic Health on Vascular Health
Eun-Jung Rhee
Endocrinology and Metabolism.2022; 37(1): 1. CrossRef - Changes in Patterns of Physical Activity and Risk of Heart Failure in Newly Diagnosed Diabetes Mellitus Patients
Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2022; 46(2): 327. CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - Impact of hypoglycemia at the time of hospitalization for heart failure from emergency department on major adverse cardiovascular events in patients with and without type 2 diabetes
Seon-Ah Cha, Jae-Seung Yun, Gee-Hee Kim, Yu-Bae Ahn
Cardiovascular Diabetology.2022;[Epub] CrossRef - Insulin resistance and heart failure with preserved ejection fraction. Pathogenetic and therapeutic crossroads
O. V. Tsygankova, N. E. Evdokimova, V. V. Veretyuk, L. D. Latyntseva, A. S. Ametov
Diabetes mellitus.2022; 25(6): 535. CrossRef - The association between metabolic syndrome and heart failure in middle-aged male and female: Korean population-based study of 2 million individuals
Tae-Eun Kim, Hyeongsu Kim, JiDong Sung, Duk-Kyung Kim, Myoung-Soon Lee, Seong Woo Han, Hyun-Joong Kim, Sung Hea Kim, Kyu-Hyung Ryu
Epidemiology and Health.2022; 44: e2022078. CrossRef - Diabetes and Heart Failure
Eun-Jung Rhee
The Journal of Korean Diabetes.2021; 22(1): 12. CrossRef - Prediabetes and the risk of heart failure: A meta‐analysis
Xiaoyan Cai, Xiong Liu, Lichang Sun, Yiting He, Sulin Zheng, Yang Zhang, Yuli Huang
Diabetes, Obesity and Metabolism.2021; 23(8): 1746. CrossRef - Diabetes and Heart Failure
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2021; 3(2): 21. CrossRef - Effects of Lipid Overload on Heart in Metabolic
Diseases
An Yan, Guinan Xie, Xinya Ding, Yi Wang, Liping Guo
Hormone and Metabolic Research.2021; 53(12): 771. CrossRef - Obesity Degree and Glycemic Status: Factors That Should Be Considered in Heart Failure
Hye Soon Kim
Diabetes & Metabolism Journal.2020; 44(4): 529. CrossRef - Letter: Associations among Obesity Degree, Glycemic Status, and Risk of Heart Failure in 9,720,220 Korean Adults (Diabetes Metab J 2020;44:592-601)
Darae Kim
Diabetes & Metabolism Journal.2020; 44(5): 777. CrossRef - Response: Associations among Obesity Degree, Glycemic Status, and Risk of Heart Failure in 9,720,220 Korean Adults (Diabetes Metab J 2020;44:592-601)
Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2020; 44(5): 781. CrossRef
- Association between underweight and risk of heart failure in diabetes patients
- Balsamic Vinegar Improves High Fat-Induced Beta Cell Dysfunction via Beta Cell ABCA1
- Hannah Seok, Ji Young Lee, Eun Mi Park, Se Eun Park, Jae Hyuk Lee, Seungtaek Lim, Byung-Wan Lee, Eun Seok Kang, Hyun Chul Lee, Bong Soo Cha
- Diabetes Metab J. 2012;36(4):275-279. Published online August 20, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.4.275
- 4,688 View
- 50 Download
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this study was to investigate the effects of balsamic vinegar on β-cell dysfunction.
Methods In this study, 28-week-old Otsuka Long-Evans Tokushima Fatty (OLETF) rats were fed a normal chow diet or a high-fat diet (HFD) and were provided with tap water or dilute balsamic vinegar for 4 weeks. Oral glucose tolerance tests and histopathological analyses were performed thereafter.
Results In rats fed both the both chow diet and the HFD, the rats given balsamic vinegar showed increased insulin staining in islets compared with tap water administered rats. Balsamic vinegar administration also increased β-cell ATP-binding cassette transporter subfamily A member 1 (ABCA1) expression in islets and decreased cholesterol levels.
Conclusion These findings provide the first evidence for an anti-diabetic effect of balsamic vinegar through improvement of β-cell function via increasing β-cell ABCA1 expression.
-
Citations
Citations to this article as recorded by- The herbal extract ALS-L1023 from Melissa officinalis reduces weight gain, elevated glucose levels and β-cell loss in Otsuka Long-Evans Tokushima fatty rats
Yujin Shin, Dongju Lee, Jiwon Ahn, Mijeong Lee, Soon Shik Shin, Michung Yoon
Journal of Ethnopharmacology.2021; 264: 113360. CrossRef - The Effect of Balsamic Vinegar Dressing on Protein and Carbohydrate Digestibility is Dependent on the Food Matrix
Eleonora Urbinati, Mattia Di Nunzio, Gianfranco Picone, Elena Chiarello, Alessandra Bordoni, Francesco Capozzi
Foods.2021; 10(2): 411. CrossRef - Safety and side effects of apple vinegar intake and its effect on metabolic parameters and body weight: a systematic review
Tine Louise Launholt, Christina Blanner Kristiansen, Peter Hjorth
European Journal of Nutrition.2020; 59(6): 2273. CrossRef - Nypa fruticans Wurmb. Vinegar’s Aqueous Extract Stimulates Insulin Secretion and Exerts Hepatoprotective Effect on STZ-Induced Diabetic Rats
Nor Yusoff, Vuanghao Lim, Bassel Al-Hindi, Khairul Abdul Razak, Tri Widyawati, Dwi Anggraini, Mariam Ahmad, Mohd Asmawi
Nutrients.2017; 9(9): 925. CrossRef - Cholesterol in Pancreatic β-Cell Death and Dysfunction
Rajib Paul, Amarendranath Choudhury, Sabanum Choudhury, Muhammed K. Mazumder, Anupom Borah
Pancreas.2016; 45(3): 317. CrossRef - Chemical Characteristics and Immuno-Stimulatory Activity of Polysaccharides from Fermented Vinegars Manufactured with Different Raw Materials
Dong-Su Kim, Byung Serk Hurh, Kwang-Soon Shin
Journal of the Korean Society of Food Science and Nutrition.2015; 44(2): 191. CrossRef - Effect and mechanisms of action of vinegar on glucose metabolism, lipid profile, and body weight
Eleni I Petsiou, Panayota I Mitrou, Sotirios A Raptis, George D Dimitriadis
Nutrition Reviews.2014; 72(10): 651. CrossRef - Chemical Property and Macrophage Stimulating Activity of Polysaccharides isolated from Brown Rice and Persimmon Vinegars
Dong-Su Kim, Kwang-Soon Shin
The Korean Journal of Food And Nutrition.2014; 27(6): 1033. CrossRef - Vinegar ingestion at mealtime reduced fasting blood glucose concentrations in healthy adults at risk for type 2 diabetes
Carol S. Johnston, Samantha Quagliano, Serena White
Journal of Functional Foods.2013; 5(4): 2007. CrossRef
- The herbal extract ALS-L1023 from Melissa officinalis reduces weight gain, elevated glucose levels and β-cell loss in Otsuka Long-Evans Tokushima fatty rats
- Retrospective Analysis on the Efficacy, Safety and Treatment Failure Group of Sitagliptin for Mean 10-Month Duration
- Won Jun Kim, Cheol-Young Park, Eun Haeng Jeong, Jeong Youn Seo, Ji Soo Seol, Se Eun Park, Eun Jung Rhee, Won Young Lee, Ki Won Oh, Sung Woo Park, Sun Woo Kim
- Diabetes Metab J. 2011;35(3):290-297. Published online June 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.3.290
- 4,307 View
- 31 Download
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background To investigate the clinical results of sitagliptin (SITA) and the characteristics of the treatment failure group or of low responders to SITA.
Methods A retrospective study of type 2 diabetic patients reviewed 99 cases, including 12 treatment failure cases, who stopped SITA because of worsening patients' condition, and 87 cases, who continued treatment over five visits (total 9.9±10.1 months) after receiving the prescription of SITA from December 2008 to June 2009. Subjects were classified as five groups administered SITA as an initial combination with metformin (MET), add-on to metformin or sulfonylurea, and switching from sulfonylurea or thiazolidinedione. The changes in HbA1c level from the first to last visit (ΔHbA1c) in treatment maintenance group were subanalyzed.
Results The HbA1c level was significantly reduced in four groups, including initial coadministration of SITA with metformin (ΔHbA1c=-1.1%,
P <0.001), add-on to MET (ΔHbA1c=-0.6%,P =0.017), add-on to sulfonylurea (ΔHbA1c=-0.5%,P <0.001), and switching from thiazolidinedione (ΔHbA1c=-0.3%,P =0.013). SITA was noninferior to sulfonlyurea (ΔHbA1c=-0.2%,P =0.63). There was no significant adverse effect. The treatment failure group had a longer diabeties duration (P =0.008), higher HbA1c (P =0.001) and fasting plasma glucose (P =0.003) compared to the maintenance group. Subanalysis on the tertiles of ΔHbA1c showed that low-response to SITA (tertile 1) was associated with a longer diabetes duration (P =0.009) and lower HbA1c (P <0.001).Conclusion SITA was effective and safe for use in Korean type 2 diabetic patients. However, its clinical responses and long-term benefit-harm profile is yet to be established.
-
Citations
Citations to this article as recorded by- Development of a 13C Stable Isotope Assay for Dipeptidyl Peptidase-4 Enzyme Activity A New Breath Test for Dipeptidyl Peptidase Activity
Roger Yazbeck, Simone Jaenisch, Michelle Squire, Catherine A. Abbott, Emma Parkinson-Lawrence, Douglas A. Brooks, Ross N. Butler
Scientific Reports.2019;[Epub] CrossRef - Characterization of changes in HbA1c in patients with and without secondary failure after metformin treatments by a population pharmacodynamic analysis using mixture models
Yoko Tamaki, Kunio Maema, Makoto Kakara, Masato Fukae, Ryoko Kinoshita, Yushi Kashihara, Shota Muraki, Takeshi Hirota, Ichiro Ieiri
Drug Metabolism and Pharmacokinetics.2018; 33(6): 264. CrossRef - Effects of 6-Month Sitagliptin Treatment on Insulin and Glucagon Responses in Korean Patients with Type 2 Diabetes Mellitus
Hae Kyung Yang, Borami Kang, Seung-Hwan Lee, Hun-Sung Kim, Kun-Ho Yoon, Bong-Yun Cha, Jae-Hyoung Cho
Diabetes & Metabolism Journal.2015; 39(4): 335. CrossRef - Clinical Characteristics and Metabolic Predictors of Rapid Responders to Dipeptidyl Peptidase-4 Inhibitor as an Add-on Therapy to Sulfonylurea and Metformin
Ye An Kim, Won Sang Yoo, Eun Shil Hong, Eu Jeong Ku, Kyeong Seon Park, Soo Lim, Young Min Cho, Kyong Soo Park, Hak Chul Jang, Sung Hee Choi
Diabetes & Metabolism Journal.2015; 39(6): 489. CrossRef - Letter: Predictive Factors for Efficacy of Dipeptidyl Peptidase-4 Inhibitors in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2015;39:342-7)
Ye An Kim
Diabetes & Metabolism Journal.2015; 39(5): 444. CrossRef - Optimal Candidates for the Switch from Glimepiride to Sitagliptin to Reduce Hypoglycemia in Patients with Type 2 Diabetes Mellitus
Hyun Min Kim, Jung Soo Lim, Byung-Wan Lee, Eun-Seok Kang, Hyun Chul Lee, Bong-Soo Cha
Endocrinology and Metabolism.2015; 30(1): 84. CrossRef - One-year real-life efficacy of sitagliptin revealed importance of concomitant pioglitazone use in Japanese patients with type 2 diabetes mellitus
Ayako Suzuki, Nakayuki Yoshimura, Yamato Mashimo, Maiko Numakura, Yuko Fujimaki, Tomomi Maeda, Toshio Ishikawa, Shin Fujimori, Kazuhiro Eto
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2013; 7(3): 143. CrossRef - Clinical Characteristics of the Responders to Dipeptidyl Peptidase-4 Inhibitors in Korean Subjects with Type 2 Diabetes
Tae Jung Oh, Hye Seung Jung, Jae Hyun Bae, Yeong Gi Kim, Kyeong Seon Park, Young Min Cho, Kyong Soo Park, Seong Yeon Kim
Journal of Korean Medical Science.2013; 28(6): 881. CrossRef - Factors predicting therapeutic efficacy of combination treatment with sitagliptin and metformin in type 2 diabetic patients: the COSMETIC study
Soo Lim, Jee Hyun An, Hayley Shin, Ah Reum Khang, Yenna Lee, Hwa Young Ahn, Ji Won Yoon, Seon Mee Kang, Sung Hee Choi, Young Min Cho, Kyong Soo Park, Hak Chul Jang
Clinical Endocrinology.2012; 77(2): 215. CrossRef
- Development of a 13C Stable Isotope Assay for Dipeptidyl Peptidase-4 Enzyme Activity A New Breath Test for Dipeptidyl Peptidase Activity
- The Association of Unintentional Changes in Weight, Body Composition, and Homeostasis Model Assessment Index with Glycemic Progression in Non-Diabetic Healthy Subjects
- Eun-Jung Rhee, Ji-Hun Choi, Seung-Hyun Yoo, Ji-Cheol Bae, Won-Jun Kim, Eun-Suk Choi, Se Eun Park, Cheol-Young Park, Seok Won Park, Ki-Won Oh, Sung-Woo Park, Sun-Woo Kim, Won-Young Lee
- Diabetes Metab J. 2011;35(2):138-148. Published online April 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.2.138
- 3,801 View
- 39 Download
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We performed a retrospective longitudinal study on the effects of changes in weight, body composition, and homeostasis model assessment (HOMA) indices on glycemic progression in subjects without diabetes during a four-year follow-up period in a community cohort without intentional intervention.
Methods From 28,440 non-diabetic subjects who participated in a medical check-up program in 2004, data on anthropometric and metabolic parameters were obtained after four years in 2008. Body composition analyses were performed with a bioelectrical impedance analyzer. Skeletal muscle index (SMI, %) was calculated with lean mass/weight×100. Subjects were divided into three groups according to weight change status in four years: weight loss (≤-5.0%), stable weight (-5.0 to 5.0%), weight gain (≥5.0%). Progressors were defined as the subjects who progressed to impaired fasting glucose or diabetes.
Results Progressors showed worse baseline metabolic profiles compared with non-progressors. In logistic regression analyses, the increase in changes of HOMA-insulin resistance (HOMA-IR) in four years presented higher odds ratios for glycemic progression compared with other changes during that period. Among the components of body composition, a change in waist-hip ratio was the strongest predictor, and SMI change in four years was a significant negative predictor for glycemic progression. Changes in HOMA β-cell function in four years was a negative predictor for glycemic progression.
Conclusion Increased interval changes in HOMA-IR, weight gain and waist-hip ratio was associated with glycemic progression during a four-year period without intentional intervention in non-diabetic Korean subjects.
-
Citations
Citations to this article as recorded by- Increased Risk of Nonalcoholic Fatty Liver Disease in Individuals with High Weight Variability
Inha Jung, Dae-Jeong Koo, Mi Yeon Lee, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Endocrinology and Metabolism.2021; 36(4): 845. CrossRef - Effects of nutritional supplementation on glucose metabolism and insulin function among people with HIV initiating ART
Hiwot Amare, Mette F. Olsen, Henrik Friis, Pernille Kæstel, Åse B. Andersen, Alemseged Abdissa, Daniel Yilma, Tsinuel Girma, Daniel Faurholt-Jepsen
BMC Nutrition.2021;[Epub] CrossRef - The ratio of estimated average glucose to fasting plasma glucose level as an indicator of insulin resistance in young adult diabetes
Jun Guo, Sisi Lei, Yu Zhou, Congqing Pan
Medicine.2020; 99(40): e22337. CrossRef - Reduced Skeletal Muscle Volume and Increased Skeletal Muscle Fat Deposition Characterize Diabetes in Individuals after Pancreatitis: A Magnetic Resonance Imaging Study
Andre E. Modesto, Juyeon Ko, Charlotte E. Stuart, Sakina H. Bharmal, Jaelim Cho, Maxim S. Petrov
Diseases.2020; 8(3): 25. CrossRef - Insulin resistance increases the risk of incident type 2 diabetes mellitus in patients with non‐alcoholic fatty liver disease
Yuya Seko, Yoshio Sumida, Saiyu Tanaka, Kojiroh Mori, Hiroyoshi Taketani, Hiroshi Ishiba, Tasuku Hara, Akira Okajima, Atsushi Umemura, Taichiro Nishikawa, Kanji Yamaguchi, Michihisa Moriguchi, Kazuyuki Kanemasa, Kohichiroh Yasui, Shunsuke Imai, Keiji Shim
Hepatology Research.2018;[Epub] CrossRef - Use of Novel High-Protein Functional Food Products as Part of a Calorie-Restricted Diet to Reduce Insulin Resistance and Increase Lean Body Mass in Adults: A Randomized Controlled Trial
Carol Johnston, Barry Sears, Mary Perry, Jessica Knurick
Nutrients.2017; 9(11): 1182. CrossRef - Gender differences in the association between food insecurity and insulin resistance among U.S. adults: National Health and Nutrition Examination Survey, 2005–2010
Junxiu Liu, Yong-Moon Mark Park, Seth A. Berkowitz, Qingwei Hu, Kyungdo Han, Andrew Ortaglia, Robert E. McKeown, Angela D. Liese
Annals of Epidemiology.2015; 25(9): 643. CrossRef - 1,5-Anhydroglucitol Is Associated with Early-Phase Insulin Secretion in Chinese Patients with Newly Diagnosed Type 2 Diabetes Mellitus
Xiaojing Ma, Yaping Hao, Xiang Hu, Yuqi Luo, Zixuan Deng, Jian Zhou, Yuqian Bao, Weiping Jia
Diabetes Technology & Therapeutics.2015; 17(5): 320. CrossRef - Serum glycated albumin as a new glycemic marker in pediatric diabetes
Ji Woo Lee, Hyung Jin Kim, Young Se Kwon, Yong Hoon Jun, Soon Ki Kim, Jong Weon Choi, Ji Eun Lee
Annals of Pediatric Endocrinology & Metabolism.2013; 18(4): 208. CrossRef - The Association of Maximum Body Weight on the Development of Type 2 Diabetes and Microvascular Complications: MAXWEL Study
Soo Lim, Kyoung Min Kim, Min Joo Kim, Se Joon Woo, Sung Hee Choi, Kyong Soo Park, Hak Chul Jang, James B. Meigs, Deborah J. Wexler, Noel Christopher Barengo
PLoS ONE.2013; 8(12): e80525. CrossRef - Relative contributions of insulin resistance and β‐cell dysfunction to the development of Type 2 diabetes in Koreans
C.‐H. Kim, H.‐K. Kim, E. H. Kim, S. J. Bae, J.‐Y. Park
Diabetic Medicine.2013; 30(9): 1075. CrossRef - Body Mass Index and Waist Circumference According to Glucose Tolerance Status in Korea: The 2005 Korean Health and Nutrition Examination Survey
Hye Mi Kang, Dong-Jun Kim
Journal of Korean Medical Science.2012; 27(5): 518. CrossRef - The Relationship between β-cell Function and Nutrient Intakes in Korean Adult - Using 4thKorea National Health and Nutrition Examination Survey 2009 -
You Mi Lee, Hye Kyung Chung, Heejin Kimm, Sun Ha Jee
Korean Journal of Community Nutrition.2012; 17(2): 243. CrossRef - The ratio of glycated albumin to glycated haemoglobin correlates with insulin secretory function
Daham Kim, Kwang J. Kim, Ji H. Huh, Byung‐Wan Lee, Eun S. Kang, Bong S. Cha, Hyun C. Lee
Clinical Endocrinology.2012; 77(5): 679. CrossRef
- Increased Risk of Nonalcoholic Fatty Liver Disease in Individuals with High Weight Variability
- The Cutoff Value of HbA1c in Predicting Diabetes in Korean Adults in a University Hospital in Seoul.
- Ji Cheol Bae, Eun Jung Rhee, Eun Suk Choi, Ji Hoon Kim, Won Jun Kim, Seung Hyun Yoo, Se Eun Park, Cheol Young Park, Won Young Lee, Ki Won Oh, Sung Woo Park, Sun Woo Kim
- Korean Diabetes J. 2009;33(6):503-510. Published online December 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.6.503
- 2,904 View
- 30 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Glycated hemoglobin (HbA1c) levels represent a 2~3 month average of blood glucose concentration. The use of HbA1c as a diagnostic tool for diabetes is gaining interest. Therefore, we determined the cutoff point of HbA1c for predicting abnormal glucose tolerance status in non-diabetic Korean subjects. METHODS: We analyzed the data from 1,482 subjects without diabetes mellitus in whom a 75-g oral glucose tolerance test (OGTT) was performed due to suspected abnormal glucose tolerance. We obtained an HbA1c cutoff point for predicting diabetes using Receiver Operating Characteristic (ROC) curve analysis. RESULTS: A cut-off point of 5.95% HbA1c yielded sensitivity of 60.8% and specificity of 85.6%, respectively, for predicting diabetes. There was a difference in HbA1c cut-off value between men and women, 5.85% and 6.05%, respectively. CONCLUSION: To use the cut-off point of 5.95% HbA1c for predicting undiagnosed diabetes in Koreans may be reliable. However, studies of different ethnic groups have reported disparate HbA1c cut-off points. Thus, ethnicity, age, gender, and population prevalence of diabetes are important factors to consider in using elevated HbA1c value as a tool to diagnose diabetes. -
Citations
Citations to this article as recorded by- The Cutoff Value of HbA1c in Predicting Diabetes and Impaired Fasting Glucose
Seyoung Kwon, Youngak Na
The Korean Journal of Clinical Laboratory Science.2017; 49(2): 114. CrossRef - Role of HbA1c in the Screening of Diabetes Mellitus in a Korean Rural Community
Jae Hyun Kim, Gun Woo Kim, Mi Young Lee, Jang Yel Shin, Young Goo Shin, Sang Baek Koh, Choon Hee Chung
Diabetes & Metabolism Journal.2012; 36(1): 37. CrossRef - Impact of HbA1c Criterion on the Detection of Subjects with Increased Risk for Diabetes among Health Check-Up Recipients in Korea
Hong-Kyu Kim, Sung-Jin Bae, Jaeone Choe
Diabetes & Metabolism Journal.2012; 36(2): 151. CrossRef - The Utility of HbA1c as a Diagnostic Criterion of Diabetes
Hee-Jung Kim, Eun Young Choi, Eal Whan Park, Yoo Seock Cheong, Hong-Yoen Lee, Ji Hyun Kim
Korean Journal of Family Medicine.2011; 32(7): 383. CrossRef - 2011 Clinical Practice Guidelines for Type 2 Diabetes in Korea
Seung-Hyun Ko, Sung-Rea Kim, Dong-Joon Kim, Seung-Joon Oh, Hye-Jin Lee, Kang-Hee Shim, Mi-Hye Woo, Jun-Young Kim, Nan-Hee Kim, Jae-Taik Kim, Chong Hwa Kim, Hae Jin Kim, In-Kyung Jeong, Eun-Kyung Hong, Jae-Hyoung Cho, Ji-Oh Mok, Kun-Ho Yoon
Diabetes & Metabolism Journal.2011; 35(5): 431. CrossRef - 2011 Clinical Practice Guidelines for Type 2 Diabetes in Korea
Seung-Hyun Ko, Dong-Joon Kim, Seung-Joon Oh, Hye-Jin Lee, Kang-Hee Shim, Mi-Hye Woo, Jun-Young Kim, Nan-Hee Kim, Jae-Taik Kim, Chong Hwa Kim, Hye Jin Kim, In-Kyung Jeong, Eun-Gyoung Hong, Jae-Hyoung Cho, Ji-Oh Mok, Kun-Ho Yoon, Sung-Rea Kim
Journal of Korean Diabetes.2011; 12(4): 183. CrossRef
- The Cutoff Value of HbA1c in Predicting Diabetes and Impaired Fasting Glucose
- Effects of Adding omega-3 Fatty Acids to Simvastatin on Lipids, Lipoprotein Size and Subspecies in Type 2 Diabetes Mellitus with Hypertriglyceridemia.
- Won Jun Kim, Chang Beom Lee, Cheol Young Park, Se Eun Park, Eun Jung Rhee, Won Young Lee, Ki Won Oh, Sung Woo Park, Dae Jung Kim, Hae Jin Kim, Seung Jin Han, Hong Keum Cho
- Korean Diabetes J. 2009;33(6):494-502. Published online December 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.6.494
- 2,556 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
omega-3 fatty acids are known to improve lipid profiles, the distribution of lipoprotein subclasses, and secondary prevention against post-myocardial infarction. Rare reports have emerged of synergistic results of omega-3 fatty acids with simvastatin in cases of type 2 diabetes mellitus with hypertriglyceridemia. The purpose of this study was to determine the combined relationship of omega-3 fatty acids plus simvastatin on lipid, lipoprotein size and the types of subspecies. METHODS: This randomized, multi-center, comparison study evaluated eight weeks of combination therapy (omega-3 fatty acids (Omacor) 4 g/day plus simvastatin 20 mg/day) or monotherapy (simvastatin 20 mg/day) for at least six weeks in 62 diabetic patients. Subjects with a triglyceride concentration of more than 200 mg/dL were eligible for inclusion. RESULTS: No significant differences for omega-3 fatty acids + simvastatin versus simvastatin alone were observed for triglycerides (-22.7% vs. -14.3%, P = 0.292), HDL peak particle size (+2.8% vs. -0.4%, P = 0.076), LDL mean particle size (+0.4% vs -0.1%, P = 0.376) or LDL subspecies types, although the combination therapy showed a tendency toward lower triglycerides, larger HDL, and LDL particle sizes than did the monotherapy. There were no significant differences between the two groups in regard to HDL-C, LDL-C, or HbA1c levels. There were no serious adverse events and no abnormalities in the laboratory values associated with this study. CONCLUSION: omega-3 fatty acids were a safeform of treatment in hypertriglyceridemic patients with type 2 diabetes mellitus. But, regarding efficacy, a much larger sample size and longer-term follow-up may be needed to distinguish between the effects of combination therapy and monotherapy.
- Insulin Resistance and PPARgamma.
- Bong Soo Cha, Se Eun Park
- Korean Diabetes J. 2006;30(5):317-323. Published online September 1, 2006
- DOI: https://doi.org/10.4093/jkda.2006.30.5.317
- 1,779 View
- 17 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - No abstract available.
-
Citations
Citations to this article as recorded by- Caulerpa okamuraeethanol extract improves the glucose metabolism and insulin sensitivityin vitroandin vivo
Chul-Min Park, Laxmi Sen Thakuri, Dong-Young Rhyu
Journal of Applied Biological Chemistry.2021; 64(1): 89. CrossRef - Impacts of High Sodium Intake on Obesity-related Gene Expression
Minjee Lee, Miyoung Park, Juhee Kim, Soyoung Sung, Myoungsook Lee
Journal of the East Asian Society of Dietary Life.2018; 28(5): 364. CrossRef
- Caulerpa okamuraeethanol extract improves the glucose metabolism and insulin sensitivityin vitroandin vivo
- Clinical Characteristics of Non-obese, Adult-onset Diabetes Requiring Insulin Treatment.
- Se Eun Park, Wan Sub Shim, Mi Young Do, Eun Seok Kang, Yumie Rhee, Chul Woo Ahn, Sung Kil Lim, Kyung Rae Kim, Hyun Chul Lee, Bong Soo Cha
- Korean Diabetes J. 2005;29(6):557-565. Published online November 1, 2005
- 1,081 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The aim of this study is to clarify the clinical characteristics of non-obese, adult-onset diabetes requiring insulin treatment and to compare the different characteristics of the three groups categorized according to diabetes classification. METHODS: Total 128 diabetic patients who were non-obese (BMI < 25kg/m2) and had been diagnosed with diabetes after 20 years old, requiring insulin treatment were enrolled in the study. We divided the patients into three groups : 56 patients with type 1, 37 with unclassifiable, and 35 with type 2 diabetes. The type of diabetes was assigned by comparing serum C-peptide concentration and clinical phenotypes. RESULTS: Type 2 and unclassifiable diabetes had no differences in BMI, the interval to use insulin, daily insulin dose, the level of HDL cholesterol and the positive rate for GAD Ab, but type 1 diabetes didn't. However, type 1 diabetes and unclassifiable group was lower prevalence of microvascular complications than type 2 diabetes (retinopathy 38.2, 52.8, 84.8 % ; nephropathy 37.7, 36.7, 74.2 % ; neuropathy 36.7, 36.7, 72.7 %, P<0.05). The prevalence of macrovascular complications was higher in the order of type 1, unclassifiable, and type 2 diabetes (11.1, 29.4, 72.7 %, respectively, all P<0.05). CONCLUSION: The clinical characteristics were similar between unclassifiable and type 2 diabetes, but the prevalence of microvascular complication in unclassifiable group had no significant difference compared with type 1 diabetes. The prevalence of macrovascular complications was significantly higher in the order of type 1, unclassifiable, and type 2 diabetes.
- Clinical Meaning of Postprandial Insulin Secretory Function in Korean Type 2 Diabetes Mellitus.
- Wan Sub Shim, Soo Kyung Kim, Hae Jin Kim, Se Eun Park, Eun Seok Kang, Yu Mie Rhee, Chul Woo Ahn, Sung Kil Lim, Kyung Rae Kim, Hyun Chul Lee, Bong Soo Cha
- Korean Diabetes J. 2005;29(4):367-377. Published online July 1, 2005
- 1,168 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Impaired pancreatic beta-cell responsiveness is associated with type 2 diabetes mellitus. Postprandial insulin deficiency is closely related with fasting plasma glucose, HbA1c and insulin responses to meals, but most studies examining postprandial beta-cell responsiveness have been limited by the small number of type 2 diabetic patients examined. The aim of this study was to evaluate fasting and postprandial insulin secretions in relation to the duration of diabetes, BMI and glycemic control in a large number of patients with variable disease durations. METHODS: We evaluated the fasting plasma glucose, insulin, C-peptide, HbA1c, BMI, postprandial 2 hour glucose, insulin and C-peptide in 1,170(male 662, female 508, age 54.6+/-1.6 years, duration of diabetes 5.2+/-6.3 years, BMI 25.4+/-3.3kg/m(2)) type 2 diabetic patients. The delta C-peptide, delta insulin, fasting(M0) and postprandial(M1) pancreatic beta-cell responsiveness were also calculated. The subjects were divided into three groups according to their duration of diabetes, BMI, and fasting and postprandial C-peptide levels. After adjusting for age, sex and BMI, the correlation of diabetes and HbA1c were correlated parameters. RESULTS: In the group of patients whose duration of diabetes was longer than 10 years, the BMI, fasting, postprandial and delta C-peptide, and M0 and M1 were significantly lower, but age, fasting and postprandial glucose, as well as HbA1c were significantly higher than those in the other groups. There were no significant differences in the fasting and postprandial glucose and HbA1c according to their fasting C-peptide tertiles. However, in the group of patients with the highest postprandial C-peptide tertile, the fasting and postprandial glucose and HbA1c were significantly lower than those in the other groups. The duration of diabetes, after adjustment of age, sex and BMI, was negatively correlated with the fasting, postprandial and delta C-peptide, M0 and M1, but was positively correlated with the fasting and postprandial 2 hour glucose and HbA1c. The HbA1c after adjustment of age, sex and BMI, was positively correlated with duration of diabetes, and fasting and postprandial glucose, but was negatively correlated with fasting postprandial and delta C-peptide, M0 and M1. CONCLUSION: Although the fasting and postprandial insulin secretions were decreased with duration of diabetes, the decrease in the postprandial insulin secretion was more prominent. The postprandial pancreatic responsiveness may be a more important factor in predicting glycemic control in Korean type 2 diabetic patients than the fasting pancreatic responsiveness.

 KDA
KDA
 First
First Prev
Prev





